One size doesn't fit all
In the United States, we’ve been taught that our weight corresponds with our health. And by that formula, if you are large, you are unhealthy.
Not true.
You might be surprised to learn that Body Mass Index (BMI)—the tool many of us encounter at doctor’s visits to classify our bodies as underweight, healthy, overweight or obese—is actually a poor indicator of health.
BMI is the ratio of your body weight relative to your height, squared. What it doesn’t tell you is body composition, including muscle mass, fat mass and bone density. And when you dig into the history of BMI, it’s highly problematic and not useful for individual care. Classifications were created by a 17th century mathematician, based solely on White European men in the 1800s.
According to this index, a BMI between 25 and 30 is overweight, and a BMI > 30 is obese. But to be overweight or obese by these standards does not automatically mean that you are unhealthy.
Research shows that there are more reliable measures of health than BMI, including fasting blood glucose, blood pressure, cholesterol, triglycerides, and cardiorespiratory fitness tests. Yet BMI is still the default in most health care settings.
Widespread assumptions about obesity and health have contributed to anti-fatness, or weight stigma, which have real world consequences for fat individuals and their health care experiences.
Anti-fatness shows up everywhere in our society, including clinics and exam rooms. If you are heavier, you’ve likely wrestled with ill-fitting exam gowns and too-tight blood pressure cuffs, or encountered scales that cannot accurately measure your weight. Anti-fatness also results in providers misdiagnosing clients and missing serious health conditions based on preconceived notions about health relating to body size.
At Health Care for the Homeless, our providers are working to adopt a better health-centered framework to assess and promote wellbeing called Health at Every Size (HAES). The HAES framework was developed by fat activists in the 1960s and eventually trademarked by the Association on Size Diversity and Health in 2010. It asserts, as its name suggests, that health is achievable at every size and that deviating from “normal” weight is not inherently bad.
This year, we’re taking steps to:
- Train all clinical providers on the limits of BMI and the principles of HAES. REI Health Specialist Arie Hayre-Somuah is encouraging clinicians to use an acronym she created called WAIT to combat anti-fat attitudes in real time after they weigh clients and assess BMI:
- What else is there to consider?
- Acknowledge your (anti-fat) biases.
- Inquire about your clients’ health habits, lifestyle, barriers, and facilitators to health.
- Tailor your follow up plan to your clients’ individual needs and circumstances.
- Audit our clinical spaces to assess whether medical equipment and supplies (scales, blood pressure cuffs, gowns) are size inclusive and protect the dignity of heavier clients.
- Tailor BMI screening follow-up to the clients’ needs. For example, if a person has a BMI of 40 but is otherwise healthy, we won’t automatically prescribe diet and weight loss. Instead, we’ll coach on continuing behaviors that sustain health, like exercise or drinking enough water.
As we address our biases, we believe we will build more trusting and open relationships with clients. And evidence tells us that this will mean better health outcomes, reduced weight stigma and less weight cycling and disordered eating.
Consider some common ways anti-fatness shows up in your life. Do you:
- diet before a big event?
- punish yourself for eating a sweet treat or "make up for it" with a visit to the gym?
- judge people based on their size?
- equate thinness with healthiness?
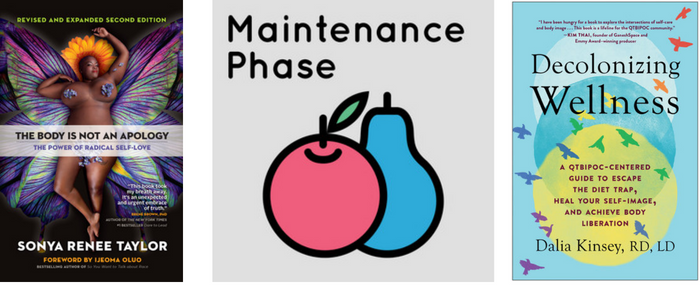
If you're interested in learning more about HAES and anti-fatness, there are a lot of resources available! You can continue debunking and unlearning anti-fat stigma by listening to the podcast Maintenance Phase or reading the work of activist and poet, Sonya Renee Taylor.
More Recent News
After a year of serving as Practice Manager of West Baltimore, Alkema Jackson is moving into the new role of Director of Practice Operations, Community Sites! She joined Health Care for the Homeless in 2022 as the Client Access Project Coordinator, collaborating across departments to help more people connect to agency services, and in 2023, she received a Core Value Award for Hope. Read on to learn more about Alkema’s approach to this new position…
Meet Christana Greene, our new Director of Compliance! With more than five years in the compliance field—most recently as Senior Quality and Patient Safety Specialist at GBMC Healthcare—Chrissy brings frontline insight to the role. She began her career as a medical assistant, gaining firsthand experience in what it takes to keep care safe and operations running smoothly. In her new role, Chrissy is focused on building a compliance culture grounded in safety, integrity and accountability. Read on to learn more about Chrissy...
Baltimore gets dangerously cold, and too many of our neighbors are out there.Here are three simple things you can do to make a difference in someone’s life this winter.
Meet Lolita Wright, a mother and caregiver. Lolita is never leaving Baltimore. She shares her parents' love of music and determination.





